Prophylaxis and therapy of diarrhea with S. boulardii
Antibiotic-associated diarrhea (AAD)
- In its current guideline, the European Society for Paediatrics (ESPGHAN) recommends S. boulardii for the treatment of acute gastro-enteritis in children.9
- As the yeast S. boulardii is insensitive to antibiotics, the prophylactic effect of S. boulardii should be used therapeutically in particular in order to minimise the risk of antibiotic-induced diarrhea.
One of the most common adverse effects of antibiotics is the development of antibiotic-associated
diarrhea (AAD). This occurs during antibiotic treatment, and even some weeks afterwards, in up to 25 % of outpatients as well as in up to 60 % of inpatients. For older, immunosuppressed and intensive care patients and/or for those requiring an extended hospital stay, the risk of AAD increases accordingly.10
The cause of AAD is usually a toxic effect of the antibiotic on the intestinal mucous membrane, as well as an imbalance of the normal gut microbiota.11 By damaging the intestinal microbiota it is possible that pathogens colonize more easily and thus overgrow the intestine. At the same time, the repeated use of antibiotics promotes the spread of pathogens with increased resistance to therapy with the applied antibiotic. The clinical picture of AAD ranges from simple diarrhea to life-threatening pseudomembranous colitis, associated with an overgrowth of Clostridium difficile in the large bowel.
Different antibiotics have a different risk of triggering AAD. There is an increased risk for cephalosporins of the 3rd generation, broad spectrum penicillins, clindamycin and clarithromycin in higher doses.
The therapeutic efficacy of S. boulardii in AAD has been confirmed in clinical trials and meta-analyses. S. boulardii reduces the frequency, the duration and severity of diarrhea associated with antibiotics.
S. boulardii reduces the risk of diarrhea in antibiotic therapy.
- This improves patient compliance and
- reduces the risk of antibiotic resistance and
- increases the success of treatment because of fewer treatment discontinuation.
S. boulardii prevents and/or reduces the occurrence of AAD in children and adults
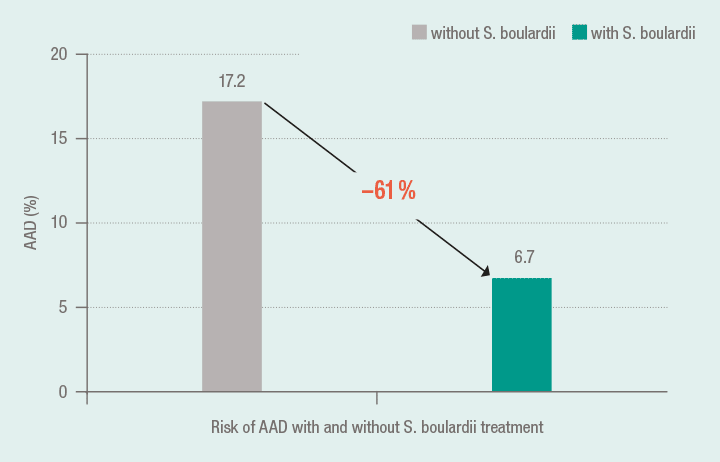
In the meta-analysis by Szajewska et al.12, the data of 1076 patients (269 children) with acute diarrhea from 5 clinical, randomised, placebo-controlled studies were evaluated. Accordingly, the risk of AAD could be lowered by using S. boulardii compared to the controls from 17.2 % to 6.7 %. Co-medication with S. boulardii with an antibiotic prevented the risk of an AAD by 61 %.13
S. boulardii halves the risk of antibiotic-associated diarrhea 12 ; 13
The very good data on the efficacy of S. boulardii in the prevention of AAD is also reflected by the positive results of the meta-analysis of McFarland14. Included in the evaluation were 10 randomised, controlled clinical trials with a total of 1858 patients. 8 studies substantiated a significant anti-diarrheal efficacy of S. boulardii in adults with AAD. The joint analysis of all 10 studies showed a reduction in the risk of diarrhea under S. boulardii by more than a half (54 %) (risk of diarrhea: S. boulardii: 8.4 %; controls: 18.4 %).
S. boulardii reduces the occurrence of AAD in hospitalised patients
In a prospective study, 151 hospitalised adults received S. boulardii in addition to an antibiotic. Only 1.4 % of patients in the S. boulardii group developed of diarrhea, in contrast to 9 % in the placebo group. This difference was statistically significant.15
9) Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, Szajewska H. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidencebased guidelines for the management of acute gastroenteritis in children in Europe: update 2014. J Pediatr Gastroenterol Nutr. 2014;59(1):132–152.
10) McFarland LV. Meta-analysis of probiotics for the prevention of antibiotic associated diarrhea and the treatment of Clostridium difficile disease. Am J Gastroenterol. 2006; 101(4):812–822.
11) Fuhr R, Stahlmann R. Gastrointestinale Nebenwirkungen von Antibiotika. Der Gastroenterologe. 2006;1:173–179.
12) Szajewska H, Mrukowicz J. Meta-analysis: non-pathogenic yeast Saccharomyces boulardii in the prevention of antibiotic-associated diarrhea. Aliment Pharmacol Ther. 2005;22(5):365–372.
13) Micklefield G. Saccharomyces boulardii in the treatment and prevention of antibiotic-associated diarrhea [Saccharomyces boulardii bei Antibiotika-assoziierter Diarrhö]. MMW Fortschr Med. 2014;156(1):18–22.
14) McFarland LV. Systematic review and meta-analysis of Saccharomyces boulardii in adult patients. World J Gastroenterol. 2010;16(18):2202– 2222.
15) Can M, Beşirbellioglu BA, Avci IY, Beker CM, Pahsa A. Prophylactic Saccharomyces boulardii in the prevention of antibiotic associated diarrhea: a prospective study. Med Sci Monit. 2006;12(4):PI19–22.
